COVID-19 DMAIC: Let in Coronavirus But Left Out Bio Science
COVID-19 DMAIC scientific Approach. While America Let in Coronavirus and Left out Bio Science, the AI-Powered Lean Six Sigma DMAIC method can help us crush the curve, save lives and get American back to work.
By Frank Shines and Umer Qureshi
August 21, 2020
“Management is prediction.”
Dr. W. Edwards Deming,
The American Who Taught the Japanese Quality
Solving complex problems is like investigating a crime scene. Whether I’m working with a tech startup, a small business, a Fortune 500 corporation, a military service branch or on a coronavirus pandemic problem, I must always listen to lots of people and follow the evidence. This means I draw upon both art and science: the art of listening, human cooperation, communication, persuasion, imagination and innovation; and the science of data, facts, processes and technologies.
Since we all learn best by doing, let’s jump right into the most real-life problem that we are all facing today — the novel coronavirus outbreak.

Rather than explaining a bunch of concepts and principles, I am going to show you how I would use the tools and apply the methods to solve the coronavirus problem. To make this accessible and understandable to the layperson, I will simplify many of the complex concepts.
Over the past 25 years I’ve worked with many of the major pharmaceutical, biologics and medical device companies in the USA and other nations to improve their business processes, analyze their data and rollout their enterprise technology systems. Recently, I’ve spent a good amount of time in biological laboratories, or biolabs, learning from the subject matter experts.
Six Sigma Approach to Examine Covid-19 (Coronavirus)
We will apply the scientific method to examining the coronavirus pandemic, using the DMAIC approach: Define, Measure, Analyze, Improve, and Control. Bill Smith and Dr. Mikel Harry developed this system, called Six Sigma, at Motorola in the 1980s. With DMAIC, we will Define the problem, Measure the current state, Analyze the root causes, Improve the process (testing on a small scale where possible), Control the gains and share lessons learned.
Because we are in the midst of the pandemic, we will not be able to fully complete this project as events evolve and data changes. For this reason, we have created a web page where updates will be provided:
First, you must clearly define the problem. Most leaders of organizations assume that people understand the problems they are solving. In my experience, they DO NOT. In nearly every case, people from different departments and even within the same departments talk “past each other.” It’s like everyone is on a different communication frequency. If you cannot explain the problem in language that everyone can understand and contribute to helping define, the problem is not fully understood.
Scientists, consultants, techies, healthcare workers, business leaders and politicians are all learning about the novel coronavirus as we go along. This is new territory for everyone – and I am no different. Data will change and findings will evolve as all of us learn more in the coming months. With that caveat, here’s how I’d approach defining the coronavirus problem.
Define the problem
Every organization is broadly made up of people, technology, processes and systems all working towards some common goal (purpose, mission, vision, strategy). The sum of organizational history and all the personalities and behaviors of the people create its culture. Culture is king. We will return to this topic shortly.
The technology consists of all of the tools, machines, data, networks, robots, software, equipment, patents, artificial intelligence algorithms, and so forth that help people do things better and faster.
The underlying “physics” of how work gets done is called the process. Smaller tasks or steps make up processes. The process of making a cup of coffee might include steps like: place coffee in filter, put filter in brewer, pour water into brewer, pour coffee into cup, and so on. Multiple processes (internal or external to an organization) come together to create a system. For example, a medical supply chain system is used to get drugs and supplies from China to hospitals in the U.S. in order to treat patients. When defining a problem, always start with the process.
Since the process helps us to define the problem, we must understand the process. As we noted earlier, the process is the real physics of how things happen or how work gets done (it is NOT some data model or a financial report) – the process is reality, what people actually do to perform their jobs.
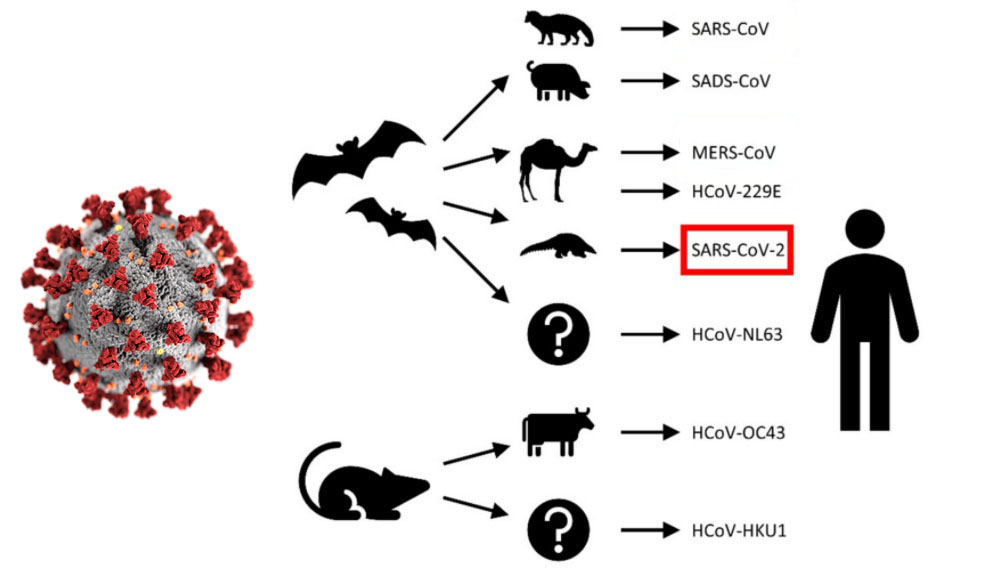
We can describe the novel coronavirus process. In simple terms, (1) the coronavirus often first jumps from a wild animal species to a domestic animal species (from bat to camel, pig or pangolin); (3) then it jumps from the domestic animal species (from a camel, pig, pangolin, etc.) to the human species; (4) finally, the virus is spread person-to-person / contact surface-to-person to more and more people.
It should be noted that we have choices. Rather than trying to stop its spread we could let the virus run its course unimpeded until we reach what is known as “herd immunity.” But this could lead to tens or even hundreds of millions of deaths.
This knowledge of the process helps us to define the first of three parts of the problem definition (“the process” itself). However, to fully define the problem we must also identify the “paint points” people feel in operational or laymen’s terms. Finally, we want to connect the problem to its “outcome” such as public health, financial results, economic output or patient impact. Here is how we might do that for the coronavirus problem:
- The process of (the “physics”) identifying, contact tracing, testing, isolating, treating and vaccinating coronavirus infected patients in our current manner
- is leading to (the “pain”) job losses, missed school and college education, economic instability, work-from-home stress and anxiety
- which has resulted in (the “human toll” / “dollars”) 2.1 million infected Americans, more than 115,000 U.S. deaths in the first 105 days, nearly 40 million Americans who filed for unemployment claims, an initial 4.8% drop in the first quarter 2020 GDP, and $6 trillion dollars of government spending to blunt the economic impact of the coronavirus crisis. [164]
We can now include a diverse set of individual voices in the conversation and seek their input. Based on that input, we might “tweak” any one or all three parts of the problem definition above. For example, medical professionals, epidemiologists, virologists, lab techs and scientists might want to change the “process” verbiage, since they are the subject matter experts of the process. Frontline emergency-response personnel, doctors, nurses and patients feel the pain the most. They might suggest revisions to the “pain-points” portion of the problem definition. Finally, doctors, medical examiners, economists, politicians and business leaders might weigh in further on the “outcomes” (deaths, dollars) section of the problem.
After receiving final input from everyone, we then make our final revisions. With the initial problem statement completed, we must now set goals, with an eye on the leading indicators or metrics that get to the core of the problem. For example, if we set a goal to increase stock market performance, without addressing the underlying public health crisis, we risk further loss of life as we provide an incentive for people to just get back to work as quickly as possible. We could then see another viral outbreak and another drop in the stock market. Therefore, our primary goal should be to first address the public health issues. Regions with minimal risk that have testing and tracing in place, we can allow to re-open much sooner. But we most closely monitor these regions with testing to remain ahead of any pending outbreak.
Here are examples of ways we may wish to define our goals. These are JUST EXAMPLES.
- Cut the current average 20,000 new cases per day by X%, from A to B by October 1, 2020
- Reduce the current three-day moving average of American deaths per day by 96%, from 2,100 deaths to 100 deaths by October 1, 2020.
- Reduce the number of unemployed workers by 25%, from X million to Y million by October 1, 2020.
- Complete testing of 120 million Americans by September 1, 2020.
- Develop and provide medical treatments (short of finding a vaccine) by September 1, 2020
- Discover a vaccine, test it and vaccinate 75% of the U.S. population by May 1, 2022
To help communicate the problem we often use a visual flowchart like a process map, or we create a SIPOC table. For simplicity I will, outline this in bullet fashion below using the SIPOC.
Suppliers (Source of the coronavirus, spread of virus)
- horseshoe bat (found in Hong Kong and mainland China)
- pangolin
- infected person expelling virus-laden droplets or mist
- surface area from which virus can be transferred to others
- surrounding air where aerosolized virus suspends, drifts
Inputs (Triggers that initiate the process)
- coronavirus jumps from horseshoe bat to pangolin
- coronavirus jumps from pangolin to humans[165]
- coronavirus spreads from human to human
- virus spreads from on porous and non-porous contact surfaces to human
Process (Steps, from infection to impact on human body)
- infected person expels virus-laden droplets
- someone else inhales the droplets; contacts surfaces then touches own face
- the novel coronavirus (SARS-CoV-2) enters the nose and throat
- CoV-2 is welcomed by cells rich in a cell-surface receptor called angiotensin-converting enzyme 2 (ACE2)
- the virus hijack’s cells, making copies and invading cells
- the infected person sheds virus in first week or so (may be pre-symptomatic or asymptomatic)
- the victim develops symptoms (fever, dry cough, sore throat, loss of smell/taste, head/body aches)
- victim’s immune system attempts to fight off the virus
- if the immune system does not fight off the virus, then the virus moves down the windpipe and attacks the lungs (can be deadly)
- the virus disrupts healthy oxygen transfer
- the white blood cell releases chemokins, summoning more immune cells (may over-react)
- immune cells target and kill virus-infected cells, leaving pus behind (pathology of pneumonia)
- pneumonia symptoms set in (coughing; fever; and rapid, shallow breathing)
- some COVID-19 patients recover breathing oxygen through nasal prongs
- other patients deteriorate, developing acute respiratory distress syndrome (ARDS)
- oxygen levels in blood fall and patient often must go onto a ventilator (only about 20% ever come off ventilator before dying, according to New York Governor Andrew Cuomo)
- the virus or body’s response to it can also harm other organs (liver, kidneys, intestines, brain, eyes, nose, heart and blood vessels); cytokine storms in which immune response goes into overdrive and attacks healthy tissues)
Outputs [166]
- damaged cells
- diminished oxygen uptake
- strokes
- seizures
- conjunctivitis
- falling blood pressure
- kidney damage
- inflammation of the eyes
- loss of sense of smell and taste
- brain inflammation
- diarrhea
- blood clots
- heart attacks
- cardiac inflammation
Customer (Patient types and human organs affected)
- patient types (elderly patients, obese patients, patients of color, patients with underlying illness, immunocompromised patients)
- lungs
- liver
- kidneys
- intestines
- brain
- eyes
- nose
- heart
- blood vessels
As we move to the next phase of our problem-solving method (Measure), we may have to return to the Define phase and make updates based on new knowledge we acquire. Don’t be concerned, this is an iterative process. Like my Express Scripts colleague, Bill S., often said:
“We reserve the right to be smarter tomorrow than we are today.”
Before discussing the Measure phase, I think this would be a good time to understand organizational culture and the psychology of change.
Primer on leading culture change
It’s been said that culture eats strategy for lunch. In my experience, it also devours execution for breakfast. While culture is probably the single most important element that affects business performance – and society at large — it is the most overlooked. You can say what you want about Steve Bannon, but the man understood the importance of culture in politics. More importantly, Bannon was smart enough to find someone who could help him convert the traditional “psychobabble” culture language of elitists and academics into practical, measurable solutions.
I was at IBM at the time Lou Gerstner “taught the elephant to dance.” That elephant was the IBM Big Blue culture, which Gerstner successfully transformed. I helped IBM enter the management consulting profession by taking principles and practical tools we developed internally to large corporations that were implementing new enterprise systems such as Oracle and SAP to address the Y2K scare. Many of the implementations by our rivals were unsuccessful. The approach we took was considered radical at the time.
First, we put the business group, not IT, in charge of the project. The business took ownership. Secondly, we embedded specific process redesign and cultural change leadership steps into the software development lifecycle. We trained the entire core team and extended team members on how to lead change. This included understanding personality preferences, conflict resolution, simple communication and marketing methods using stories, stats and analogies. We created both a “burning platform” and an optimistic vision of “building a platform for growth.” Most importantly, I spent lots of time with the executive staff explaining that culture reflects leadership style and the aggregated personalities of the organization and its history. This meant that if leaders want to change a culture, they must first change themselves.
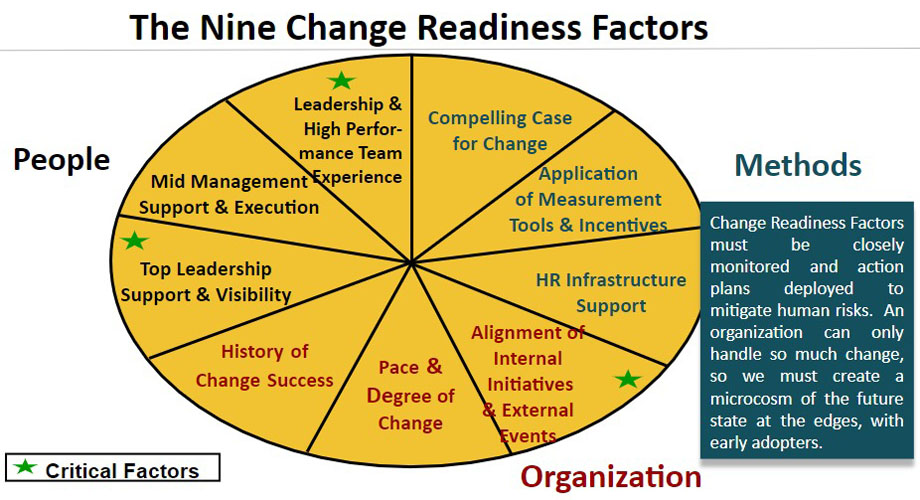
Here are key tools needed to drive sustainable culture change:
- Clearly define the gap between current state and desired future state
- The width of the gap will define how much culture change is needed
- My best tool for doing this is to use Dr. Daniel Denison’s Denison Culture Survey
- Denison’s survey will provide you with world class benchmarks and proven action plans needed to close the culture gap. Dr. Denison has linked culture traits with business and financial performance, such as sales growth, employee satisfaction, innovation, customer satisfaction, profitability.
- Understand and appreciate the importance of psychology of change and different personality types using DISC, MBTI, the OCEAN big five personality traits and/or 16personalities.com
- Create a critical mass for change by developing “micro future states” within your organization (provide early adopters with plenty of incentive – financial and non-financial based on an understanding of their personality types – to take the risk in leading change). CAUTION: Send the wrong message by firing one of these key change agents or promoting someone who is working at cross-purposes to your desired future state culture and you risk setting yourself back years as you will lose credibility and trust.
- Understand these key levers for change: HR development and coaching tools on organization design; a burning platform of the past and optimistic vision of the future; incentives, rewards, consequences; ethical, empathetic and charismatic leadership; middle management support (they can KILL everything you’re trying to do); data analysis and key performance metrics tied to HR development tools, individual performance reviews and promotional opportunities; customer, employee and culture surveys (e.g. NPS, Denison Culture Survey); communications, coaching, training and re-education programs tied to leader standard work (LSW) and standard work; an experienced core team of leaders who speak with a single voice and have been trained on project management, process and data analysis and the psychology of change.
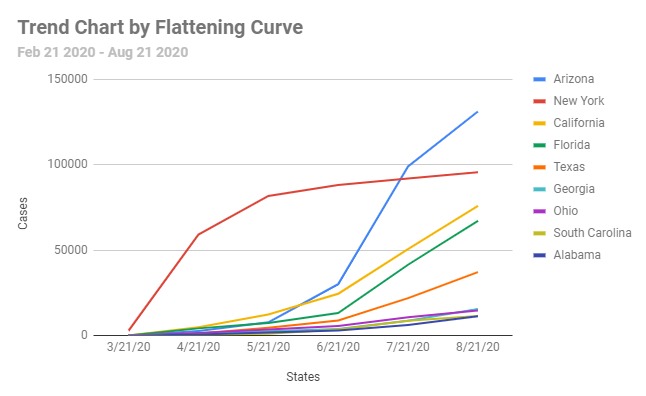
Measure current performance
In phase two, we measure the baseline performance of the process using trend lines, Pareto charts, histograms, etc. Also, we study benchmarks of leaders in our industry, different industries and around the world to make comparisons. Without a baseline measurement, we will not know if an action we’ve taken really improved the results. Also, without measurements we have no objective way of defining the problem or holding ourselves and others accountable. Consequently, political agendas, the loudest voice in the room, fake news and conspiracy theories will come to dominate the conversation, resulting in lost time, resources and possibly in lost lives.
My mentors, Forrest Breyfogle and Drs. Mikel Harry, Kosaku Yoshida and W. Edwards Deming, are the pioneers in our industry. They taught me that data provides objectivity, but that data is NOT reality. Recall the lessons we discussed in the chapter, Situational Awareness, in which I described my pilot training days and the importance of “getting your head out of the cockpit.” The cockpit instruments are the data; looking out of the cockpit windscreen is reality. To paraphrase best-selling author and cosmologist, Stephen Hawking, “Why should the universe go through all of the trouble of obeying our equations?” In short, data is necessary but insufficient. Always augment data with reality by going to the place where things are happening and observe for yourself. Listen first and treat everyone fairly, with dignity and respect.
As we examine the measurement phase keep a couple of quotes in mind about data.
- “There is no such thing as a true figure.” – Dr. W. Edwards Deming, Quality Expert
- “The most important figures that one needs for management are unknown or unknowable, but successful management must nevertheless take account of them.” – Dr. Lloyd S. Nelson, Statistician
- “Not everything that counts can be counted, and not everything that can be counted counts.” – Albert Einstein, Physicist
Over the coming weeks and months, the world will amass more data. But as of August 28, 2020, 03:25: ET (New York Time), here is a baseline summary of some of what we know from WorldOMeters.
- Total deaths worldwide: 835,733
- Total cases (infections) worldwide: 24.6 million
- Worldwide deaths per million population: 107.2
- Worldwide cases per million population: 3,161
- Total U.S. deaths: 184,803
- Total U.S. cases: 6.0 million
- US. deaths per million population: 558 (5 times higher than worldwide metric)
- US. cases per million population: 18,256 (6 times higher than worldwide metric)
- Average number of new U.S. deaths per day: ~1,143 per day
- Average number of new U.S. cases per day: ~46,286 per day
- US. infection fatality rate (IFR): 1.3% [167]
- US case fatality rate (CFR): varied across U.S. counties, from 0.9% to 19.3% [167]
- 38 million U.S. workers filed for unemployment benefits in the first nine weeks (Jun 15, 2020)
- Number of Americans tested for coronavirus: 24.8 million (7%; est. 331 million people)
- Average time it takes to develop and approve a vaccine (historically): 6-8 years[168]
- Maximum time virus lives: 72 hours (plastic or stainless steel); 24 hours (cardboard); 4 hours (materials like copper); 3 hours (droplets hang in air before they fall)
Analyze root causes
The third phase of the DMAIC approach is Analyze. We conduct a thorough analysis of all potential sources of the root causes of the problem in order to identify short-term, mid-term and long-term countermeasures or solutions that we will implement. We do not want to be distracted by coming up with solutions for “symptoms” of the problem; otherwise the problem will simply recur at a different time, in a different department or with a different person or team.
The analysis phase is typically one of the most intense and time-consuming phases of the problem-solving method. This is where conflict often arises and it is so important to first train teams on personality types, conflict resolution and the psychology of change. However, when the analysis phase is done well, it leads to the most promising solutions being short-listed for final consideration during the Improve phase. I typically conduct multiple cross-functional workshops and Kaizen events to brainstorm and pilot-test process improvement ideas and new technologies.
We often use the 6M, fishbone Cause-and-Effect diagram created by Kaoru Ishikawa in the 1960s. The Effect would be “High number of U.S. COVID-19 deaths.” The Cause categories would be Machines, Materials, Mother Nature, Manpower/Womanpower, Methods and Measurements:
- Machines: Ventilators; High volume testing machines and low-volume testing machines (e.g., Abbott ID NOW™ COVID-19, Bosch Rapid COVID-19), computer systems, mobile apps
- Materials: Lysol disinfectant, Clorox bleach, personal protective equipment (gowns, gloves, masks, booties, face guards); collection supplies (swabs, collection tubes, lancets, alcohol swabs, transport media, infrared thermometers); lab materials to support machines such as RNA extraction kits, PCR tests (reagents, cartridges)
- Mother Nature: temperature, humidity, sunlight (UV rays), population density, geography, time zone, negative pressure rooms in hospitals
- Manpower / Womanpower: age, gender, illnesses, comorbidities, immune-compromised
- Methods: testing, contact tracing, social distancing, shelter in place, isolation / quarantine, use of masks in public.
- Measurements: cases, tests, hospitalizations, intubations, deaths, treatments, vaccines, unemployed workers, closed schools and businesses, etc.; where we are along the epidemiological curve (have we flattened or lowered the curve?)
A multi-disciplined team will weigh in on which of these causes are the most likely root causes of the problem. In addition to the cause and effect diagram, I often have teams use causal loops, scatterplots and the 5 Whys (asking why five times). For example: Why are so many people dying of COVID-19? Because they are getting infected by others? Why are they getting infected by others? Because they (and others) are not practicing social distancing. Why are they not practicing social distancing? Because they believe COVID-19 is no worse than the common flu? Why do they believe it’s no worse than the flu?… etc. The goal here is to get to root causes of the problem as opposed to focusing on symptoms of the problem. This is one of the most common errors that managers and teams make. So, it bears repeating. If the team spends their time coming up with improvements for symptoms of the problem the problem will simply pop up again in a different place or at a different time. Consequently, we will waste time and money and contribute to a confused and distrustful citizenry.
Depending on the size of the group and number of root causes identified, I might facilitate agreement using a simple team-voting system to rank the most likely causes. This gives us a manageable short list of items on which we can focus. We then brainstorm potential solutions to address each of the root causes. To get team members to think “outside-of-the-box” and come up with more innovative ideas, I often suggest the team consider Dr. Edward Bono’s lateral thinking methods or Six Thinking Hats. I also show teams how to apply the 40 Principles of TRIZ (theory of inventive problem solving) to come up with creative solutions. With a list of potential solutions in hand we then move to the Improve phase. [169].
Improve the process
During the Improve phase of DMAIC, we decide which solutions from our list we will implement and in which order. Once again, this is an iterative process. We may find that once we tally up all of the potential solutions and their impact, we can only achieve 70 percent of our goal. If so, we will have to return to previous phases in order to brainstorm other ideas and identify additional solutions to close that 30 percent gap.
We are ready to now create our Improvement Matrix (Impact vs. Effort). Impact is shown on the vertical axis and represents Benefits (to reduce the number of COVID-19 cases and deaths). Effort is displayed on the horizontal axis and represents time, resources and costs (the dollar value or the number of weeks, months or years to implement an improvement). Team members now write each potential solution on a sticky note and place it on the wall for all to see. Each solution is put on the matrix to show its relative position to other solutions, weighing its benefits (impact) against its effort.
Solutions that have a high benefit and require the least effort become candidates for short term solutions that give us the ‘biggest bang for the buck.” We delegate to a sub team that then develops a detailed plan. The sub-team then shares that plan with the larger group for final review and agreement. The sub team also starts pilot-testing ideas as quickly as possible to determine if there are potential risks and to identify if there are any unforeseen consequences. They conduct this pilot working very closely with frontline workers at the grass-root level (for example, onsite at the hospitals with nurses and in the biolabs with med techs).
We repeat this approach for mid-term and long-term solutions, which might also involve coordinating with other countries and international institutions.
A list of solutions to implement, would be broken down as shown:
Short-Term Improvements (takes a week to three months): Gets you 25% of your goal
- Wash hands frequently for at least 20 seconds, use paper towel to shut off faucet and open doors
- Clean surfaces and carry germicide and cleansing wipes on your person to use whenever needed
- Wear masks in public
- Maintain social distance of six feet from others when in public
- Isolate high-risk individuals (elderly and immune-compromised) from low-risk individuals (youth)
- Keep social gatherings to 10 people or less
- Shelter-in-place (only go outside of your home for essential items such as food, medication, etc.)
- Conduct baseline microbe mapping data collection (scientists take air samples and swab samples of public contact surfaces like subways, ATMs, benches, etc.)[170]
Mid-Term (takes four to eleven months): Gets you another 40% of your goal
- Complete COVID-19 (virus, not antibodies) testing of “X” million Americans per week
- Conduct passive disease surveillance and microbe mapping data analysis as part of early warning detection (air and swab samples of public areas)
- Complete contact tracing and isolation of those identified
- Find, test and rollout pre-vaccine therapies and other treatments
- Provide incentives and consequences for communities to comply with public health guidelines
- Provide ongoing communication to the public and adjust as required based on science and in consideration of human nature and human psychology
- Partner with hi-tech and consulting companies to develop innovative methods for working from home and redesigning workplaces to comply with public health guidelines and regulators such as OSHA, FDA, etc.
- Identify low-risk individuals and communities then develop options for slowly allowing people to return to work, school, college (comply with public health guidelines, monitor outcomes with data, and adjust appropriately; consider hybrid models of in-person and online learning; be prepared to return to shelter in place as outcomes dictate)
Long-Term (will take more than a year): Gets you another 30% of your goal; just shy of total 100%
- Develop, test and rollout COVID-19 vaccine(s)
- Share data, coordinate and work with other countries on COVID-19 vaccinations
- Provide incentives and consequences for communities to comply with public health guidelines
- Provide ongoing communication to the public and adjust as required based on science and in consideration of human nature and human psychology
- Partner with hi-tech and consulting companies to develop innovative methods for working from home and redesigning workplaces to comply with public health guidelines and regulators such as OSHA, FDA, etc.
- Identify low-risk individuals and communities then develop options for slowly allowing people to return to work, school, college (comply with public health guidelines, monitor outcomes with data, and adjust appropriately; consider hybrid models of in-person and online learning; be prepared to return to shelter in place as outcomes dictate)
It is far too early to know which improvements will prove to be successful and to what degree and by what date. For this reason, please follow developments here:
https://letinbutleftout.com/covid-19-dmaic/
Control gains and celebrate our heroes
We have reached the final phase of the DMAIC model, the Control phase. The purpose of the control phase is to ensure gains made to “flatten the curve” and reduce the number of daily COVID-19 cases and deaths is maintained. Additionally, we want to celebrate success, honor our heroes and capture and share lessons learned.
We are too early in the pandemic life cycle so, once again, I will refer you to the link below where we will continue to track developments and update findings.
https://letinbutleftout.com/covid-19-dmaic/
In this chapter we have applied the DMAIC scientific problem-solving method to the current coronavirus pandemic. Any organizational leader can apply this DMAIC approach to help guide teams on complex problem solving that gets to the underlying root causes, rather than fire-fighting symptoms.
